Agent Action Plan
Big changes are ahead for the ACA, and as you get ready for plan year 2026, a little early prep can make a big difference.
That’s why we created this Agent Action Plan: to help you stay ahead of the curve, keep your clients covered, and make the most of the new tools in HealthSherpa. It’s designed to support you through every step of your pre-OEP workflow, so you can reconnect with your book of business, work more efficiently, and set yourself up for a successful enrollment season.
.png)
WHAT TO PLAN FOR
OE 2026 will be different. Expect to:
- Actively renew your entire book of business, including those clients that would passively renew (auto-renew) in a typical year
- Spend more time on the enrollment process for most clients
- Collect documentation prior to Open Enrollment
- Engage early with clients and create a dialog before OE begins
This year, many consumers who would have passively renewed in previous years will need more support. Start your OE prep by reviewing your entire client list.
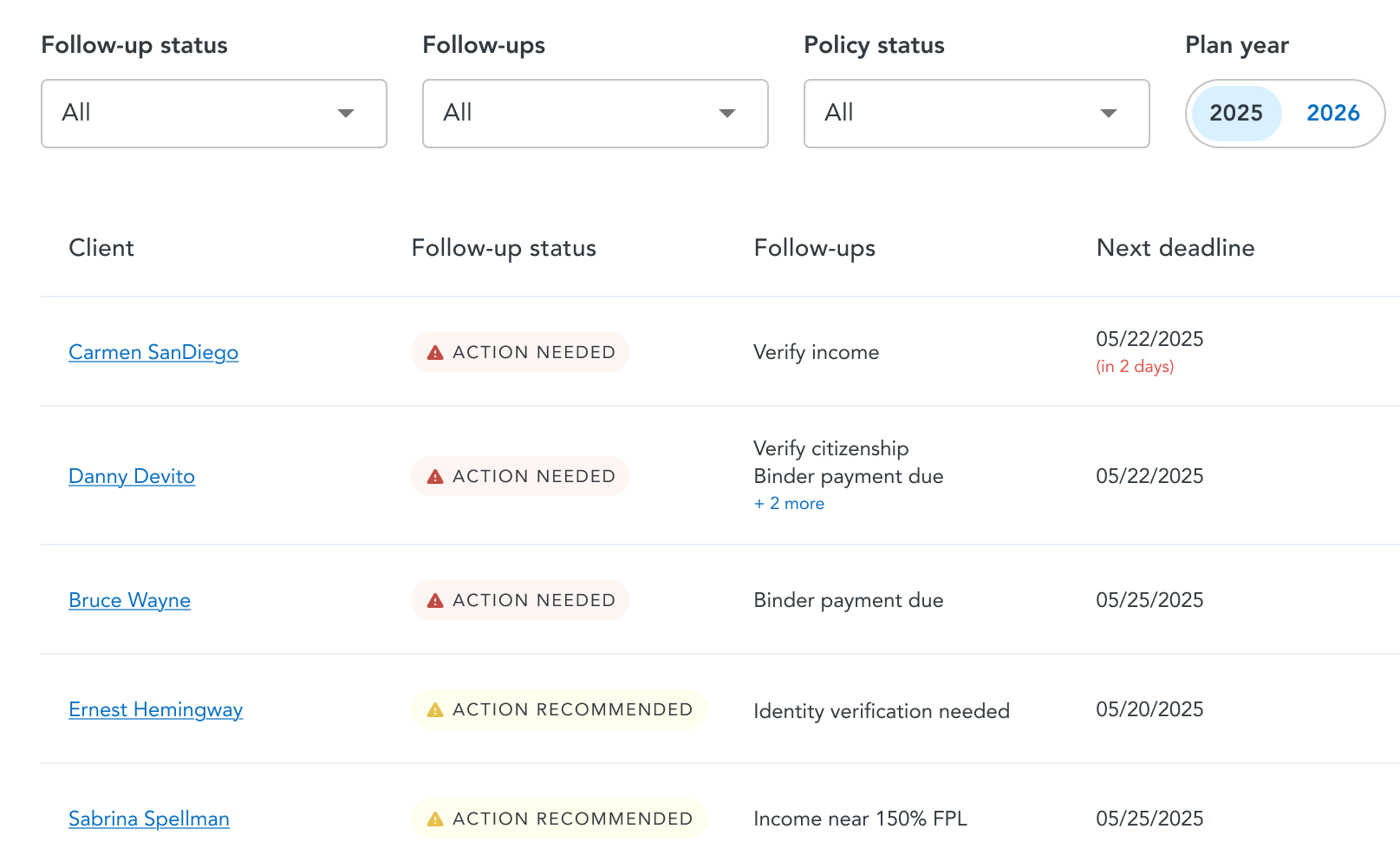
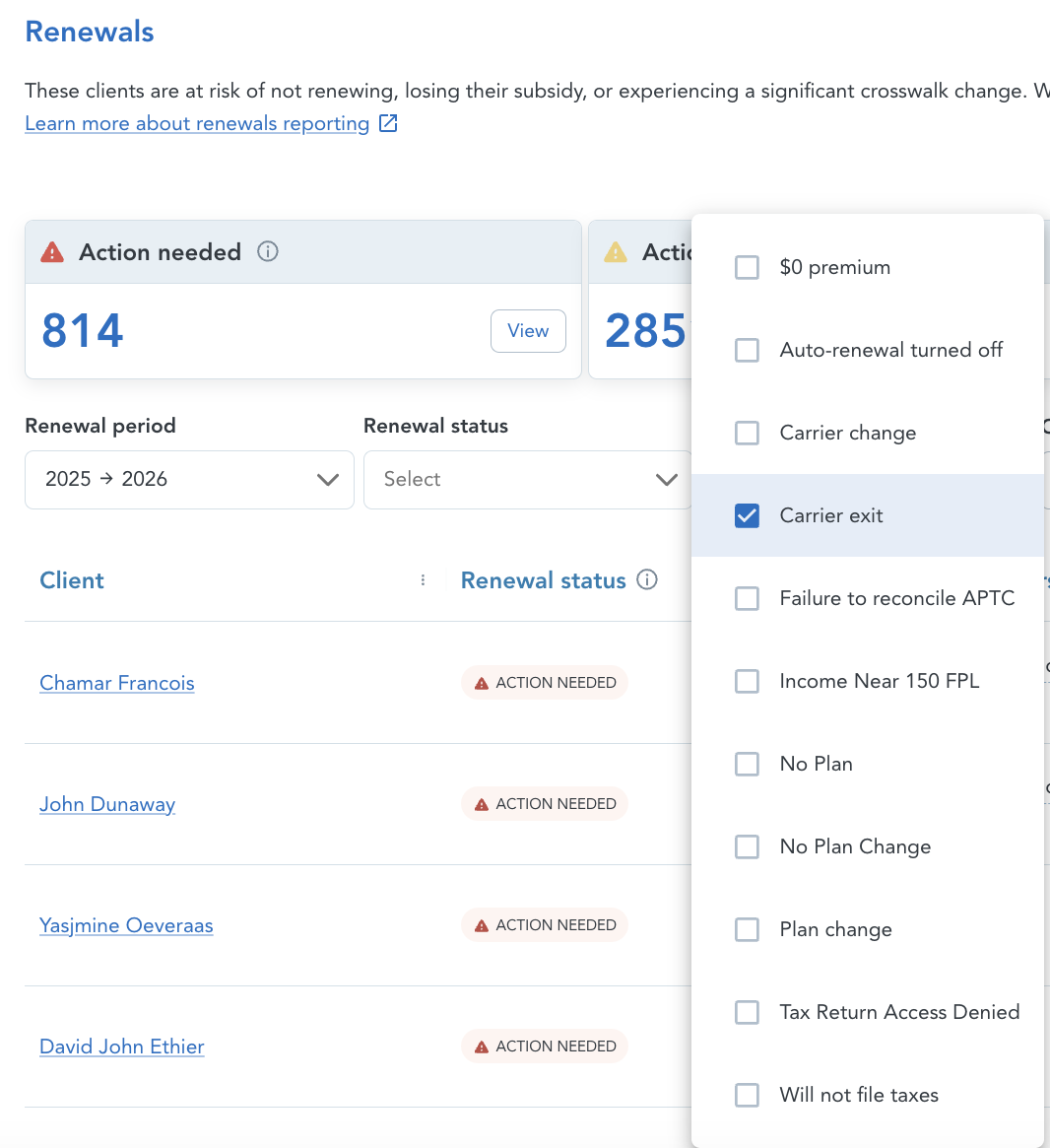
In HealthSherpa, you can view your client list along with DMIs, SVIs, payment status, and renewal factors to prioritize your outreach strategy for OE26:
- Client follow-ups tab: See all follow-ups for each client in one place, making it easier to prioritize your work. Policies requiring action and with the soonest deadlines appear at the top of the list. You can also export a filtered list to perform and track outreach on specific follow-ups.
- Renewal factors have been added to help you identify clients affected by ACA changes, such as:
- Income near 150 FPL
- Income near 400 FPL
- $5 monthly payment
- Tax return access denied
- Failure to reconcile APTC
- Carrier exit
HealthSherpa's Client follow-ups tab:
Refresher course on active vs passive renewals:
It’s important to start engaging with your clients early. Doing so helps you educate and retain them, while also giving you the chance to collect information and documentation ahead of time. By having these details ready before November 1, you’ll free up more time during Open Enrollment to focus on completing enrollments.
During early outreach, explain that to remain covered in 2026 consumers may need to provide additional information and/or review plans.
Learn about uploading follow-up documents
Learn about managing consent with HealthSherpa
Live agent training:
Follow-up documentation and collecting documentation early
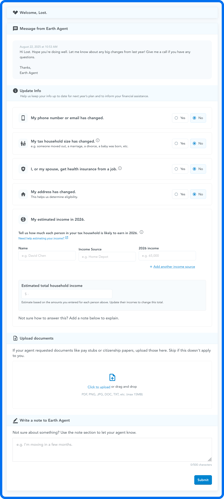
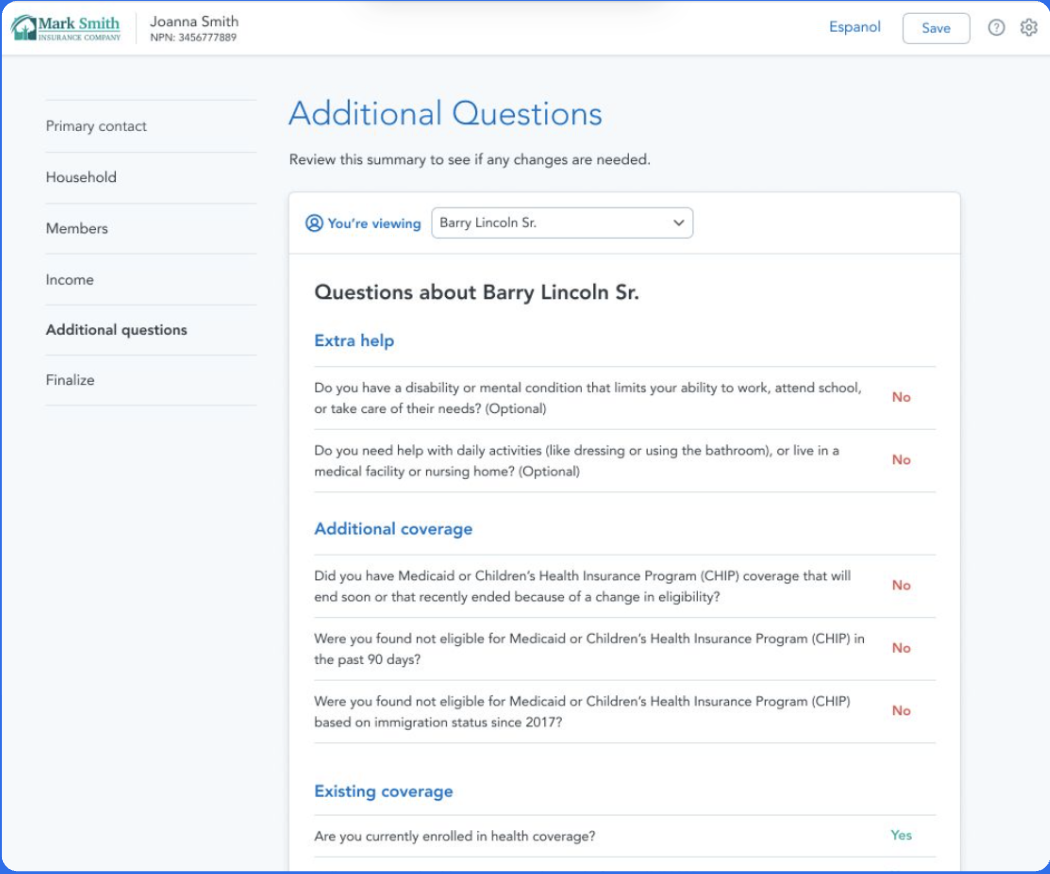
Start Intake now, save time during OE.
Use the Share intake link to pre-collect the information you’ll need for client renewals. Start sending your clients secure links to share updated household details, income adjustments, uploaded documents, and even notes back to you. You’ll find the secure Share intake link from the Clients page and Documents due tab.
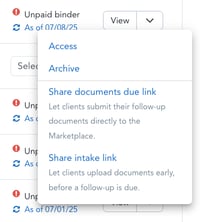
All client submissions will appear on the Intake tab on your Clients page for easy tracking and organization.
Later, when you are renewing your consumer during OE, you'll be able to see the consumer's Intake form side-by-side with the application.
HealthSherpa's Renewal Intake form:
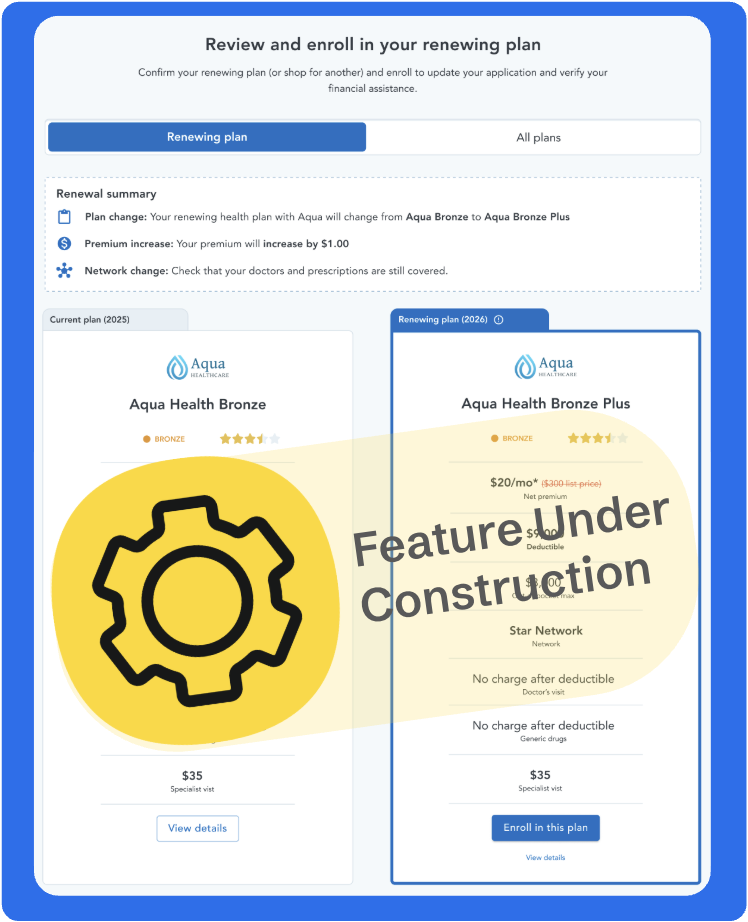
When Window Shopping begins, compare plans with your clients
This year, once Window Shopping opens, you’ll be able to see your consumer’s current plan next to the crosswalk plan for 2026.
This gives you a head start to review changes, compare options, and help your client make a decision so they’re ready to enroll as soon as Open Enrollment begins.
Once OEP begins, leverage renewal factors to prioritize your active renewals
Leverage the renewal factors and prioritization you established prior to OE to begin processing active renewals.
Renew consumers quickly
Renewals will be even faster this year with updates that allow you to:
- Go directly to sections of application that need changes.
- Skip lengthy clicks and CMS wait times during application for info that doesn’t change.
SEP CHANGES
The Special Enrollment Period is ending for clients with ≤150% FPL
- New clients may no longer be SEP eligible beginning in May, and they will need a qualifying life event (QLE) to enroll outside of OEP.
- Educate your team about all available QLEs so they are ready to explore alternative SEP opportunities with consumers.
Prepare to supply SEP pre-enrollment verification
- For SEP enrollments, expect to submit documentation to verify your client’s QLE.
- If the Marketplace can’t verify your client’s QLE, they may lose their SEP eligibility.
Read the SEP Overview to learn about
- Special Enrollment Period (SEP)
- Qualifying Life Events (QLEs)
- DMIs and SVIs
Not on HealthSherpa?
Create a free agent account or request a demo for your agency!
.png)
